Your Pre-Surgery Class is scheduled on:
Date: Monday
Time: 1:30 pm to 2:45 pm
Place: Microsoft Teams (Virtual class)
*Note: The in-person class is cancelled at this time.
This class was created to help patients with breast cancer to:
- Know what to expect during and after breast cancer surgery
- Speak with and meet other patients having surgery
- Prepare for the day of their surgery.
You are welcome to bring one guest.
To attend the pre-surgery class, call your surgeon’s office assistant to arrange a date to attend the class before your surgery.
- If you would like to attend this class in your language, call 416 581 8604. Ask for a medical interpreter to translate this class. This is a free service. Please call at least 5 business days before the class.
If you are not able to attend the class or would like to hear the information again, please watch the videos:
If you have any questions about the class, call the surgical coordinator at 416 946 4501 extension 4302.
Who do I contact for more information?
If you have questions about your surgery or recovery, call the Surgical Nurse Specialist (CNS) at 416 946 4501 extension 4302. If you are not able to reach the Surgical Nurse Specialist, call the Breast Clinic Triage Nurse at 416 946 2228 (Breast Clinic Hotline).
Call your surgeon to book appointments or confirm your surgery date at:
- Dr. Tulin Cil: 416 946 4501 extension 3984
- Dr. Andrea Covelli: 416 586 4800 extension 5164
- Dr. Alexandra Easson: 416 586 4800 extension 2775
- Dr. Jaime Escallon: 416 586 4800 extension 5163
- Dr. Wey-Liang Leong: 416 946 4501 extension 2992
- Dr. David McCready: 416 946 4501 extension 6510
- Dr. Michael Reedijk: 416 946 4501 extension 4432
Call your doctor or nurse right away if you notice any of these signs:
- Nausea (wanting to throw up) that does not go away
- Vomiting (throwing up) that does not go away
- Bleeding that does not stop in the area that had surgery
- Surgery area getting very red
- Foul smelling drainage (fluid coming out of the area that had surgery)
- Pus coming out of the incision (cut made during surgery)
- Fever higher than 38 °C (100.4 °F)
- Area that had surgery is swollen and hard, or firm
- Your drain falls out (if you have a drain)
If you notice any of these signs on a weekend or at night, go to a walk-in clinic. Tell the hospital staff at the front desk that you had a breast surgery.
What is breast cancer surgery?
Breast cancer surgery is any surgery on the breast(s) to try to remove cancer. There are 2 main types of breast cancer surgery:
- Lumpectomy (surgery to remove a part of the breast)
- Mastectomy (surgery to remove the whole breast)
Both a lumpectomy and mastectomy, when done for cancer, usually include surgery to remove some of your lymph nodes. Lymph nodes are small, bean-shaped vessels that are found all over your body, including under your arms (see page 9 to learn more about lymph nodes).
The cost of all breast cancer surgeries is paid for by the Ontario Health Insurance Plan (OHIP).
Read the next section to learn about lumpectomy and mastectomy surgery.
What is a lumpectomy?
A lumpectomy is surgery to remove a lump in the breast, and some breast tissue in the area around it. The amount of tissue removed depends on the size of the lump.
Sometimes, a lumpectomy is also called a:
- partial mastectomy
- wide excision
- wedge excision
- excisional biopsy
The goal of a lumpectomy is to remove the lump (tumour) and try to prevent the spread of cancer.
This image shows a lump (tumour) being removed during a lumpectomy.
What happens during a lumpectomy?
There are 5 main steps in having a lumpectomy:
- You may need Molli seed put into your breast to help guide your surgeon to the area being removed. This process is called “seed localization” and is usually used for small lesions. Your surgeon will talk to you about this if needed. The seed localization step happens while you are awake, and is likely done on another day before the surgery. You should not have pain with this procedure as you will have local freezing to numb the breast before the marker is placed into the breast.
- Your doctors will give you general anesthetic (medication to help you relax and sleep through the surgery). You will already have an IV (intravenous). A breathing tube will be put in while you are asleep.
- When the lump is found, an incision (cut made during surgery) is made and the lump and some tissue around it are removed.
- The incision is closed with stitches. These stitches will dissolve on their own and will be covered with a skin tape called “Steri-Strips”. A bandage will be used to cover the whole area.
- The breast tissue removed during surgery is sent to a pathologist (a doctor who tests body tissue to see if disease is there).
A lumpectomy with lymph node surgery can take up to 1.5 hours (90 minutes).
What is a mastectomy?
A “mastectomy” is surgery to remove the whole breast, usually including the nipple.
Sometimes, a mastectomy is also called a:
- simple mastectomy
- total mastectomy
The goal of a mastectomy is to remove the cancer in the breast and to try prevent the spread of cancer.

This image shows the part of the breast that is removed during a mastectomy, and where your lymph nodes are.
What happens during a mastectomy?
There are 5 main steps in having a mastectomy:
- Your doctors will give you general anesthetic (medication to help you relax, and sleep through the surgery). You will already have an IV (intravenous). A breathing tube will be put in while you are asleep.
- The whole breast is removed. If you are not having breast reconstruction, this includes the nipple, areola and some skin. If you are having breast reconstruction, some skin and sometimes the nipple and areola are kept.
- The breast tissue removed during surgery is sent to a pathologist (a doctor who tests body tissue to see if disease is there).
- One or 2 tubes, called “drains”, are placed under the incision (cut made during surgery).
Drains help to remove fluid from the surgery area and prevent swelling. Swelling is caused by fluid buildup under the skin.
To learn more about drains see page 20.

The image shows you where the drain will be placed.
- The incision is closed with stitches. These stitches will dissolve on their own and will be covered with a skin tape called “Steri-Strips”. A bandage will be used to cover the whole area.
A mastectomy with lymph node surgery can take up to 2 hours. If both breasts are removed or if there is breast reconstruction, the surgery will take longer.
What is lymph node surgery?
Your lymphatic system removes extra fluid and waste from your body. It plays a major role in how your immune system (protects your body from disease) works.
- Your lymphatic system is made up of lymph nodes that are linked by lymph vessels.
- Your lymph nodes are bean-shaped vessels that are found all over your body. Large groups or chains of lymph nodes can be found in your neck, under your arms and in your groin.
- Lymph node surgery is when lymph nodes are removed and tested to see if cancer has spread there. During a lumpectomy or mastectomy, lymph nodes are often removed from the area under your arm during the same surgery.
The lymphatic system: Circles show where groups of lymph nodes are in your body. It is normal for lymph nodes to be removed during breast cancer surgery.
The lymph nodes under your arm, on the side you had surgery, are some of the lymph nodes that will be removed and tested.
Why do people have lymph node surgery?
The goal of this type of surgery is to remove certain lymph nodes in your armpit.
Lymph node surgery is important because it can help your health care team to:
- Find out if cancer has spread to the lymph nodes in your armpit
- Remove cancer that has spread to your armpit
What are the types of lymph node surgeries?
There are 2 types of lymph node surgery:
- Sentinel lymph node biopsy
- Axillary lymph node dissection
Talk to your surgeon to know:
- If you need lymph node surgery
- Which option is best for you
Read the next section to learn about each type of surgery.
What is a sentinel lymph node biopsy?
A biopsy is when a small sample of tissue or cells from your body are removed and tested to see if there is disease there.
The goal of a sentinel node biopsy is to remove 1 to 5 lymph nodes and test them. The type of lymph node removed during this surgery is called a sentinel lymph node.
Sentinel lymph nodes are the first lymph nodes that cancer cells are likely to spread to. Removing and testing the sentinel lymph nodes helps your health care team to know if the cancer has spread from the breast.
What happens during a sentinel lymph node biopsy?
Before your surgery:
Using a needle, a dye (gives out low amounts of radiation) is put into the area of your breast having surgery. This dye is injected (put) into the lump on your breast using imaging.
You will get about 2 to 4 needles. The needles may feel like a bee sting for about 60 seconds or less.
You will have the dye injected at the hospital you are having surgery at any time from 30 minutes to 24 hours before your surgery.
During your surgery:
- Using a needle, you will be given a second dye (called the “blue dye”) which is injected around your nipple. The second dye is used to highlight the lymph nodes that drain from your breast first.
After getting the needle, your urine (pee) may be blue for a few days and you may notice some blue around the injection site, which will fade with time. - Using a probe that can find radiation and visual cues, your surgeon will be able to find the sentinel lymph nodes.
- When the sentinel nodes are found, your surgeon will remove them. The nodes will be sent to the pathologist.
- The incision is closed with stitches. These stitches will dissolve on their own. They are covered with a skin tape called “Steri-Strips”. A bandage is used to cover the whole area.
If you are having a lumpectomy at the same time, you will likely get a second incision (cut made during surgery) in your armpit to remove the sentinel nodes. If you are having a mastectomy the surgeon will likely use the same incision.

These images show you how a sentinel lymph node biopsy is done, and where the sentinel lymph nodes are removed from.
If you are having a frozen section on the sentinel nodes, then they will be rapidly checked by the pathologist when you are asleep. If cancer is found, the surgeon will do an axillary node dissection.
What about localized nodes?
If you are having a lymph node localized, Molli seed is put into your breast a day or more before your surgery. An ultrasound is used to guide the seed along with local freezing (numbing medicine). The surgeon removes the localized node and sentinel nodes at the time of surgery.
What is an axillary lymph node dissection?
The goal of an axillary lymph node dissection is to remove lymph nodes from your axilla (area in your armpit). This is done when it is known that there are some cancer cells that have moved to your underarm.
There are often between 10 and 30 lymph nodes removed from the area under your armpit. This number is different for every person.
Axillary lymph nodes may need to be removed so your pathologist can test them to know how much the cancer has spread there from your breast and remove it.
What happens during an axillary lymph node dissection?
- During the surgery, many of the axillary lymph nodes in the armpit area are removed.
- One drainage tube is placed under the incision (cut made during surgery) in your armpit area to drain the lymphatic fluid (clear-to-white fluid that moves around your lymphatic system) and blood. If you are having a mastectomy, this drain will be in the center of your chest.
- The incision is closed with stitches. These stitches dissolve on their own. They are covered with a skin tape called “Steri-Strips”. A bandage is used to cover the whole area.

These images show you how an axillary lymph node dissection is done, and where the axillary lymph nodes are removed from.
What are the risks of surgery?
Like any surgery there are risks and side effects linked to having breast surgery, such as:
You will be given medication to help you feel comfortable and manage any pain. See page 16 for details on how to manage pain.
You may also feel or notice:
- A change of feeling or less feeling (numbness) in the breast and arm that had surgery
- Swelling around the area where you had surgery. Sometimes this can feel like a golf ball under your arm.
- Stiffness in your arm on the side of the body where you had surgery
- Changes to your body image, or comfort with your sexuality. This may be because there will be changes to how your breast will look after surgery.
Get support and cope with any changes to your body image or sexuality by attending the Princess Margaret’s class on Sex & Intimacy. To attend this free class, or get more details, call 416 581 8620.
If you would like to talk to someone about any changes to your body image, ask your doctor to refer you (book a visit) to see a hospital social worker or call 416 946 4501 extension 4525.
Most side effects can last a couple weeks to a month.
How to prepare for surgery?
Do this a few weeks before your surgery:
- You will have a pre-admission appointment, which is booked by your surgeon’s office. It can be on the phone or in person.
Do this 5 days before your surgery:
- Stop taking aspirin. It can increase your risk of bleeding during surgery.
If you take a blood thinner (like Warfarin, also called Coumadin), talk to the doctor who prescribed the blood thinner and your surgeon before you stop taking it, and to know when to start taking it again.
You can start taking aspirin again 5 days after your surgery.
- Stop taking any herbal medication, supplements or remedies. This includes vitamin E, garlic pills, and fish oil pills. These may affect your surgery and treatment. It is okay to eat garlic and fish.
Talk to your doctor or nurse if you have any questions or concerns. You can start taking aspirin and herbal medications, supplements or remedies again 5 days after surgery.
Do this 2 days before your surgery:
- Stop taking anti-inflammatories like ibuprofen (Advil, Motrin). You can start taking these medications again 2 days after your surgery. It is OK to take Tylenol.
Do this the day before your surgery:
- Drink plenty of fluid the day before surgery. This includes juice, soup, water, and fluids in your food. This will help you feel less thirsty the morning of your surgery.
Do this the night before your surgery:
- Do not eat salty foods. This will help you feel less thirsty on the morning of your surgery.
- Do not eat any solid food after midnight. This includes candy or chewing gum.
- Shower using soap to lower the chance of infection.
Do this the morning of your surgery:
- Do not swallow anything 5 hours before surgery. This includes both food and drinks. For example, if your surgery is scheduled for 2:00 pm, you cannot have food or drinks after 9:00 am.
You must have an empty stomach before surgery. You can drink clear fluids up to 4 hours before your surgery. Clear fluids include: water, apple juice, ginger ale, tea and black coffee. Do not have milk or cream in any of your drinks. - Shower using soap. Do not use deodorant, perfumes or lotions on the side of your torso (stomach, chest, breast, under-arm area, and back) getting surgery. This will help you prevent infection and stay safe during surgery. It is okay to use shampoo, face cream and lotions on other parts of your body.
- Do not wear jewelry, make-up or nail polish on your fingers or toes.
- Only take the medications your health care team told you to. If you are unsure please speak to your health care team.
- Leave your valuables at home.
- Arrive at the hospital and check-in on time.
Important: Follow any other instructions your surgeon or anesthesiologist (person who gives medication to help you relax, and sleep through the surgery) gives you.
What should I bring to the hospital the day of my surgery?
- Your health card (OHIP card).
- Any medication you usually take, if you are staying overnight in the hospital. You may need to take them while in hospital.
- Slippers or shoes. You need comfortable footwear to walk around the hospital in.
- If you have sleep apnea and use a CPAP machine, please bring it to the hospital.
- Something comfortable that opens in the front to wear home, and your post-op bra if needed (more information below).
What to expect after surgery
Right after surgery, you will:
- Wake up in the recovery room. You will feel sleepy and need to rest.
- There is a waiting area nearby where your guests can wait. A member of your health care team will let your guests know when it is okay for them to see you.
- Have an intravenous (IV) in your arm. You will be getting fluids and medication through the IV.
- Have a sore throat. This is from a tube that was placed in your throat to help you breath during the surgery.
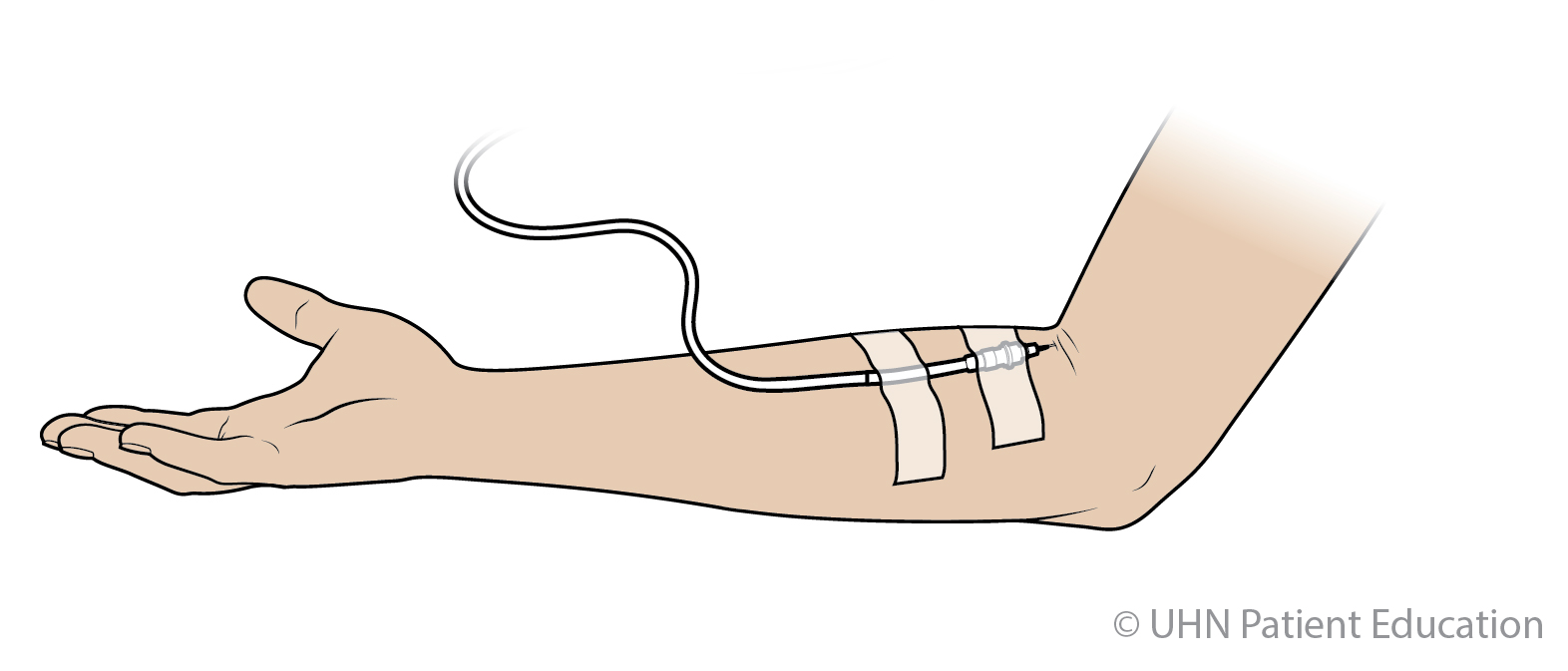
This image shows you where the IV is often inserted (put in).
For a while after surgery you may:
- Feel nauseous (feeling of having to throw-up), or vomit (throw-up)
- Feel tired
- Feel some pain or discomfort. Stay active and move around after the surgery to prevent complications (problems that can arise after surgery). Take your pain medication if it is uncomfortable to move around.
- Have some bruising and tenderness where the incision (cut made during surgery) is. You may notice this a few days after your surgery. This can last for about one month.
When can I leave the hospital?
- You will go home the same day as the surgery, unless your surgeon has given you different instructions.
- If you are having breast reconstruction using your own tissue (i.e. DIEP), talk to your nurse or surgeon about your length of stay.
How will my pain be managed?
Your doctor will give you some pain medication. Most people will get Hydromorphone (which is an opioid) and acetaminophen (Tylenol).
Take your pain medication as needed.
- If you still feel pain after taking the medication, tell your doctor or nurse. They can help you manage the pain.
- For mild pain, take acetaminophen, 325 mg (Tylenol) or acetaminophen, 500 mg (Tylenol Extra Strength). Take it every 4 to 6 hours, as needed. You could also take ibuprofen (Advil) after 2 days from the surgery.
- As your incision starts to heal, you may feel sharp jabbing pains or a tingling feeling in that area. To help with this, your doctor may prescribe (give you) a medication called Gabapentin.
Gabapentin is used to treat nerve pain. It will help to relieve or reduce your pain. Gabapentin will need to be taken the same way as the doctor prescribes (tells you to) for it to work.
What if I get constipation from my medication?
If you get constipation (not able to poop), nurse or pharmacist. They can suggest a stool softener (like colace) or laxative (like lactulose). You can buy these medications without a prescription to make it easier for you to have a bowel movement (poop). The stronger pain medications often cause this.
How do I care for my incision?
- Remove the outside dressing 2 days after surgery.
- If you had breast reconstruction, leave your dressing on until you see your plastic surgeon.
- Leave Steri-Strips (paper tapes) on for 14 days. They may fall off before 14 days. It is okay if this happens. After 14 days you can remove Steri-Strips by pulling them towards the incision.
- If you have staples, they will be removed by your community nurse.
- Do not put other lotions on the incisions until after your follow-up appointment, and your doctor says it is okay to do so.
How do I care for my drain?
If you are having a mastectomy or axillary node dissection you will have a drain. Follow the instructions below until your incision has healed.
Do this while you are healing:
- Secure the drain to your clothing. This will help prevent pulling on your skin.
- Milk the drain every 4 hours. You only need to milk the drain when you are awake. Your nurse will review how to do this right after surgery.
If the drainage stops suddenly, it may be blocked. Try milking the drain a few times to clear the blockage.
- Empty the drain 2 times a day. You can empty it more often if it becomes full.
Measure the amount of fluid you remove each time and when it was emptied. Squeeze the drain while putting the cap back on to start the suction again.
The drain will be removed after the amount of fluid is less than 30 millilitres in 24 hours for 2 days in a row.
What if there is leakage where the drain leaves my skin?
If the fluid comes out where the drain exits your skin, pat it dry. Cover the place where your drain exits your skin with gauze padding.
What do I do if the drain falls out?
- Do not panic. This very rarely happens and is not an urgent problem.
- Cover the incision where the drain left the skin with gauze. Use gauze or a bandage to soak up any drainage.
Call your Clinical Nurse Specialist to let them know what happened.
You can learn more about the drain by watching Going Home After Breast Cancer Surgery with Drains.
What if I have swelling in the area where I had surgery?
- Some soft swelling for up to one month after surgery is normal.
- It’s normal to have swelling at the breast or chest, and up to an egg-sized swelling in the armpit.
- Call your Clinical Nurse Specialist if swelling becomes hard or grows very large (see page 2 for phone numbers). Your surgeon may want to assess you (give you a check-up) in clinic.
What if I notice numbness where I had surgery?
The area where you had surgery may be numb. This often happens during the first week after surgery.
You may also feel numbness in your upper arm or behind your back.
As you heal, you will slowly gain more feeling again. During this time, it is normal to feel sharp, “jabbing” pains in the area.
You may also feel a tingling feeling. Tapping the numb area or massaging the area may help.
What if I see signs of infection?
See Call your doctor or nurse right away if you notice any of these signs on this page to learn what to do if you see any signs of infection.
What if I am bleeding from the incision?
It is normal to have a small amount of dried at the incision (cut made during surgery) site. This could be either:
- Under the Steri-Strips
- On the bandage covering the incision
Call a member of your team if you notice a large amount of fluid or blood coming from the incision site non-stop. A large amount of fluid or blood would be about half a cup to 1 cup every hour.
What if I notice a tight cord-like feeling when I move my arm or see a “cord” under my arm?
This tight feeling or “cord” can run from your armpit all the way down your arm. This is common and can take several months to get better. Continue to do your exercises and massage the area. Talk to your doctor at your appointment.
Can I take a shower after my surgery?
- For the first 2 days after surgery, have a sponge bath. Keep the area where you had the surgery dry.
- The outer bandage can be removed 48 hours after your surgery. You can then take a shower. You can shower with your drain. Avoid soaking the surgery site with water.
- If you had breast reconstruction, leave your dressing on until you see your plastic surgeon. You can still shower.
Do I need to change what I eat after surgery?
No. You can eat normally. If you are taking strong pain medications you may want to have more fibre and water in your diet (food and drinks) to prevent constipation.
Can I apply lotions to my breast or underarm?
Do not apply any of these on the side of your body where you had surgery:
- perfumed lotions
- talcum powder
- underarm deodorant
These things can irritate or bother your skin. You can start using these again once your incisions have healed. Wait until your follow-up appointment with the surgeon.
When can I drive?
- Do not drive or operate machinery if the effects of the general anesthetic (medication to help you relax and sleep through the surgery) have not worn off yet. The effects of general anesthetic may continue to cause drowsiness and dizziness even after you leave the hospital.
- After the general anesthetic, do not drink alcohol for 24 hours after your surgery. This may make your drowsiness and dizziness worse.
- Do not drive if you are taking narcotic pain medication. These medications include Tylenol 3 (Tylenol with Codeine also called acetaminophen and codeine) or hydromorphone.
These medications may make you drowsy or dizzy. If you do drive while taking these medications, you may have an accident and hurt yourself. - Do not drive if you cannot fully move your arm(s) on the side where you had the surgery.
What bra should I wear after surgery?
- If you had a lumpectomy, wear a bra without underwire for a week or two even while you sleep.
This helps from pulling on the surgery site and helps with swelling. - If you had a mastectomy, wear a comfortable shirt or a mastectomy camisole.
- You can buy camisoles and bras at The Wig Boutique on the 3rd Floor of the Princess Margaret or at most medical garment stores.
Read the pamphlet called Bra Buying Guide for Breast Cancer Patients for more details and a store list.
Ask your health care team for a copy or visit the Patient & Family Library to pick up a copy (Main floor of the Princess Margaret).
This is an image of a camisole. Breast drains can be held inside the pouches on the front, below the breasts.
What happens at my follow-up appointment?
You will have a follow-up appointment with your surgeon. It will be about 2 to 3 weeks after surgery.
Your surgeon’s assistant will give you an appointment time. They may give you a follow-up appointment time when they book your surgery date, or they may give you an appointment after you go home from surgery.
At this appointment your surgeon will:
- Check to make sure your incision is healing well
- Check to see how well your arm is moving
- Talk to you about the test results from your surgery
After this appointment, your surgeon may refer you to other health care providers. They will talk to you about any other treatments you may need.
Where can I find more general information about breast cancer?
If you would like more information, go to:
Patient & Family Library
Main atrium, Princess Margaret Cancer Centre
Phone: 416 946 4501 extension 5383
Website: Cancer Health Information
The Patient & Family Library offers trusted information about:
- cancer
- cancer treatment and care
- support organizations and services
At the Patient & Family Library you will find computer stations, books, brochures, DVDs, audio books, electronic books and CDs. Trained staff and volunteers can help with your questions and help you to find the information and resources you need.
You can also visit these websites:
